SOME STORIES IN THE HISTORY OF MEDICINE
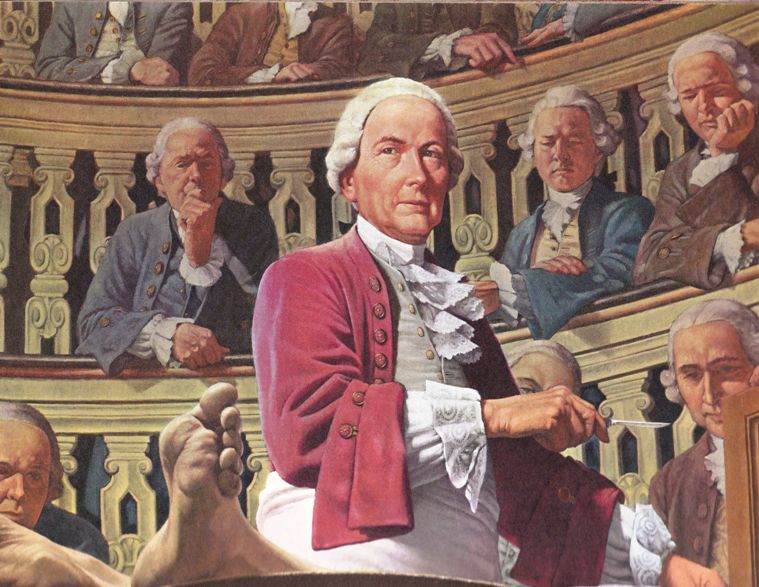
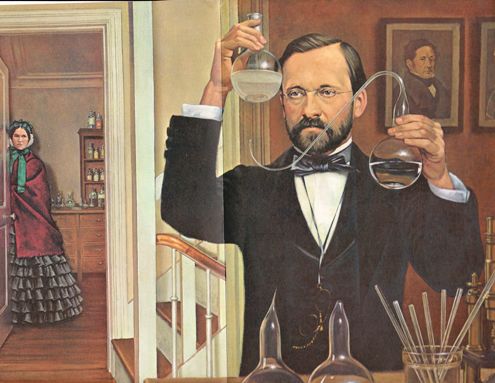
Lecture 2: Contagion, Infection, Antisepsis
Adam Blatner, M.D.
You can also click on the following links:
1. The first lecture was an introduction and some history of the microscope, laying the foundation for the other lectures.on the background
Also, three supplements, which you can click on to link to related webpages:
A. A very brief overview of the history of medicine. (pre-history to the Renaissance) (just to get you oriented)
B. Further Overview to modern times.
C. A further history of microscopy.
Then: (To be posted as I prepare and give these lectures: )
(Lecture 2 is here on this present webpage). 3: The Early History of Immunology ; 4: The Discovery of Anesthesia;
5: Recognizing Nutritional Deficiencies ; 6: Hygiene: Sanitation, Hookworm, Dental Floss, & Summary
(First Posted February 2, 2009)